What you need to know about nerve damage associated with diabetes and how it can be treated.

Over 11% of the U.S. population has diabetes. Diabetes, especially if poorly controlled, can cause a host of complications, including heart disease, blindness, and amputations. Perhaps the most common complication of diabetes is diabetic peripheral neuropathy (DPN), when small fibers become damaged from chronically high blood sugar levels. Over 50% of people with diabetes will experience the tingling, numbing, and burning pain of DPN from these small fibers not connecting and transmitting messages to the rest of the body as they should. While there is no cure for DPN once you’re diagnosed, effectively managing the related pain can help patients restore an active lifestyle.
While certain nerve medications may be prescribed, procedural-based pain relief may be your first step in eliminating DPN-related pain, rather than a last resort. “There are a lot of interventions that are not opiates or pain medications that are opportunities to take away pain that doesn’t have the risks of certain medications…so these are important attempts to alleviate pain. Eighty percent of patients can get relief from what’s out there and what medical technology has to offer,” says Thomas Kraus, DO, MBA, DAAPM of Tennessee Valley Pain Consultants, a double-board certified physician in anesthesiology and pain management.
Lumbar Sympathetic Nerve Blocks
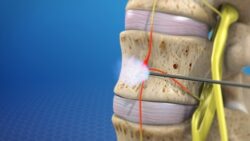
Pain associated with neuropathies is a form of sympathetic pain originating from the autonomic nervous system. We don’t have to think about the autonomic nervous system for it to work – it controls our heart beating, digestion, and breathing. A lumbar sympathetic nerve block is a steroid-free injection given into the lower part of your back (the lumbar spine). It disrupts the pain-transporting chain of your autonomic nervous system that runs from your spine up to your brain.
While medications offer around 40% pain relief for most people, a lumbar sympathetic nerve block may offer near complete relief. But how long this relief lasts varies entirely on how your body responds to the treatment. Most people receive 8 to 12 weeks of significant pain relief before needing another block. These blocks are done in the clinic in dedicated procedure suites and take about 5 minutes to complete using an x-ray device called a fluoroscope after receiving twilight sedation. The most common block is the lumbar sympathetic nerve block. This treats DPN in your legs and feet, which are the top areas to experience DPN. But if you experience DPN in your arms, a stellate ganglionic block could be an effective option.
Spinal Cord Simulators (SCS)
SCS started as a treatment for the spine but has evolved to offer relief to patients with all kinds of neuropathies, including DPN. It can be thought of as a pacemaker for your spine instead of your heart. A SCS cuts off the pathway that carries pain signals between your spine and brain that trigger pain. The patient even controls the amount of relief the device provides at any given time. An SCS can take away pain for many years. According to Dr. Kraus on SCS’s benefits, “Unfortunately in medicine, nothing is 100%. But there’s a 70% chance for profound relief for people that have intractable pain – that’s a lot; that’s really significant.”
If you and your provider agree that a SCS is a beneficial option for you, you’ll go to the clinic for a trial device to be placed, which usually takes 15-20 minutes with twilight sedation. If your pain is significantly reduced after 7 days, you could consider having a SCS permanently placed. For permanent placement, you’ll go into the operating room where a 2-inch diameter generator will be inserted under the skin of one of your buttocks. A permanent SCS needs charged every 4 to 7 days, taking 30 minutes per charging session, similar to other modern electronic devices. The rechargeable battery lasts around 7 years, meaning that you should require very few interventions in between.
How Tennessee Valley Pain Consultants Can Help
With 100 years of combined experience, the specialty physicians at Tennessee Valley Pain Consultants are the region’s leader in providing personalized pain management to maximize your quality of life. “It doesn’t hurt to come talk to a physician about what your options are. The most important part is that the patient makes a good decision about how they want to be treated—getting all your options out there to try to alleviate pain and make your life more bearable,” Dr. Kraus emphasizes.
Treating DPN-related pain should start with an open conversation with healthcare professionals who treat nerve pain like the physicians at Tennessee Valley Pain Consultants. Click here to request an appointment today.